Solutions in General and Colorectal Surgery

WITH EPIFIX®
COLOSTOMY REVERSAL WITH AMNIOFIX

Advanced Placental-Based Allografts When Patients Are in Need
Providing Protective Barriers and Environments that Support the Healing Cascade
There are many risk-factors to healing such as patient co-morbidities and complex defects.1 MIMEDX offers an array of advanced placental-based allografts that may be used in a variety of surgical applications to provide valuable benefits in patient care.
Product Advantages: AMNIOEFFECT, AMNIOFIX, and AMNIOCORD
- Provide a protective barrier and environment that supports the healing cascade
- Protect the wound bed to aid in the development of granulation tissue
- Provide a human biocompatible extracellular matrix (ECM) and contain 250+ regulatory proteins 2-5
AXIOFILL
- A lyophilized, biocompatible, and human extracellular matrix derived from the placental disc.
- For use in the replacement or supplementation of damaged or inadequate integumental tissue.
- Versatile and easy to use: apply dry or hydrated as a paste.
- Early scientific data in a nude mouse model shows AXIOFILL supports site appropriate function in tissue by allowing cell attachment, new collagen formation on the matrix, and new blood vessel formation.6
Clinical Use Examples:
- Debridement/ Dehiscence
- Complex soft tissue defects
- Complex incision management
- STSG
- Low anterior resection
- Colostomy reversal
- Fistula repair
- Amputations
Case Studies and Clinical Evidence:
How Physicians Use Our Products
Case study 1
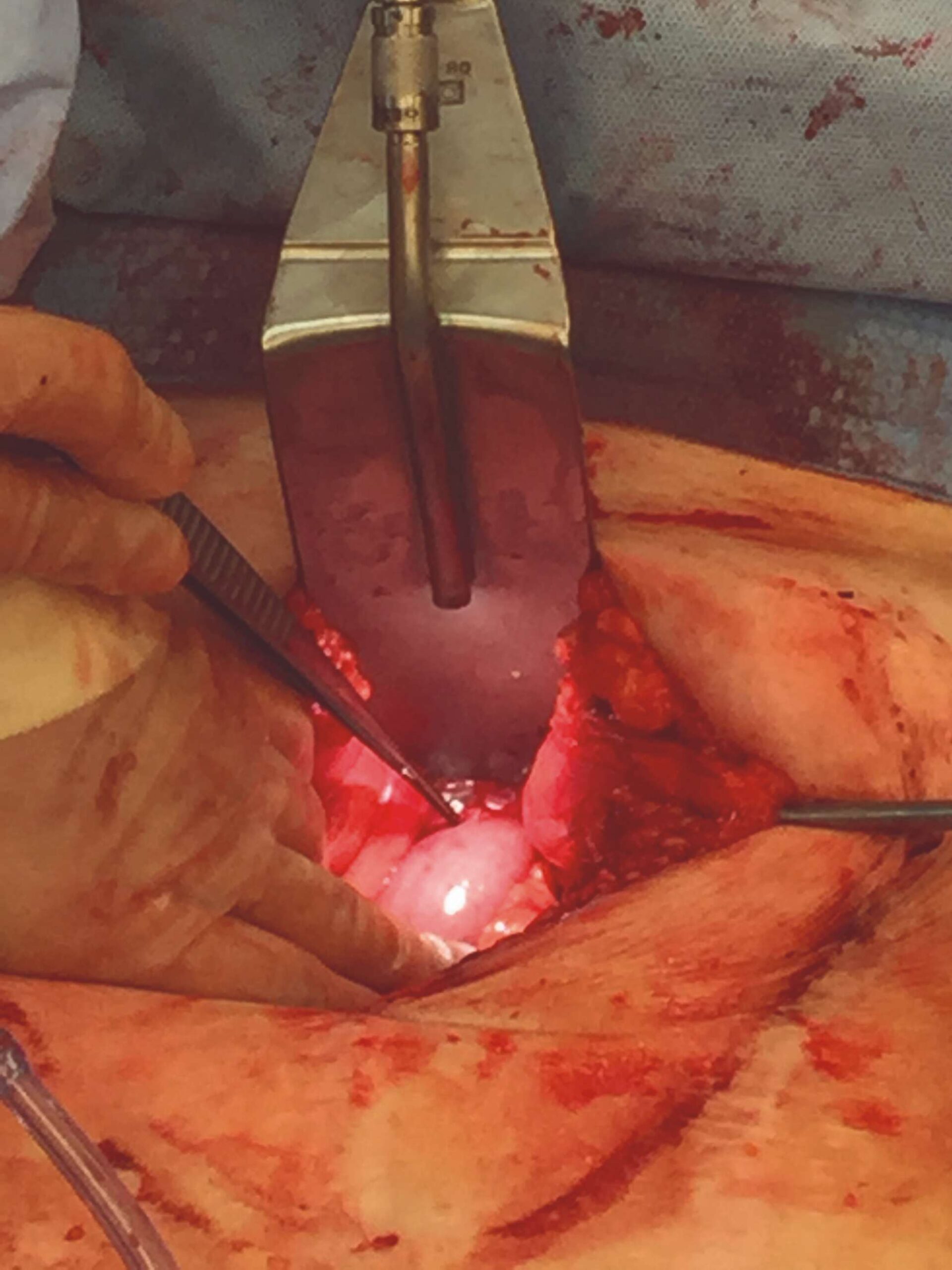
Acute Abdominal Wall Dehiscence with EPIFIX7
Challenge
A 62-year-old obese male, BMI of 29, type II diabetes, with a history of hypertension, myocardial infarction with stent placements, multiple abdominal surgeries, and over 40 years of cigarette smoking, underwent large ventral hernia repair. At one week post-op, the patient developed ischemia at the incision line, which led to an incisional dehiscence.
Studies have shown a direct correlation between the number of comorbidities and clinical outcomes. A significant rise in complications, length of stay, and mortality rates is associated with the rise in number of patient comorbidities.8-10
Surgical Intervention
The patient was managed with serial debridement and wet-to-dry dressings for two months, then placed on negative pressure wound therapy (NPWT) for four weeks at home. After one month of NPWT, the wound had only decreased by 30%. NPWT was discontinued, and EPIFIX was applied every other week, instead of weekly, due to the travel distance for the patient.
Follow-Up
Upon examination at his two month EPIFIX follow-up visit, the wound was fully closed and re-epithelialized. The patient returned for a routine one-year visit and has remained fully closed and asymptomatic.
 Following Debridement Following Debridement |
 Four weeks of NPWT, only 30% size reduction, first EPIFIX 4 cm x 4 cm applied Four weeks of NPWT, only 30% size reduction, first EPIFIX 4 cm x 4 cm applied |
 Week 2: Two 2 cm x Week 2: Two 2 cm x3 cm EPIFIX applied |
 Week 4: One 2 cm x Week 4: One 2 cm x3 cm EPIFIX applied |
 Week 8: Wound closed and stable Week 8: Wound closed and stable |
Case study 2
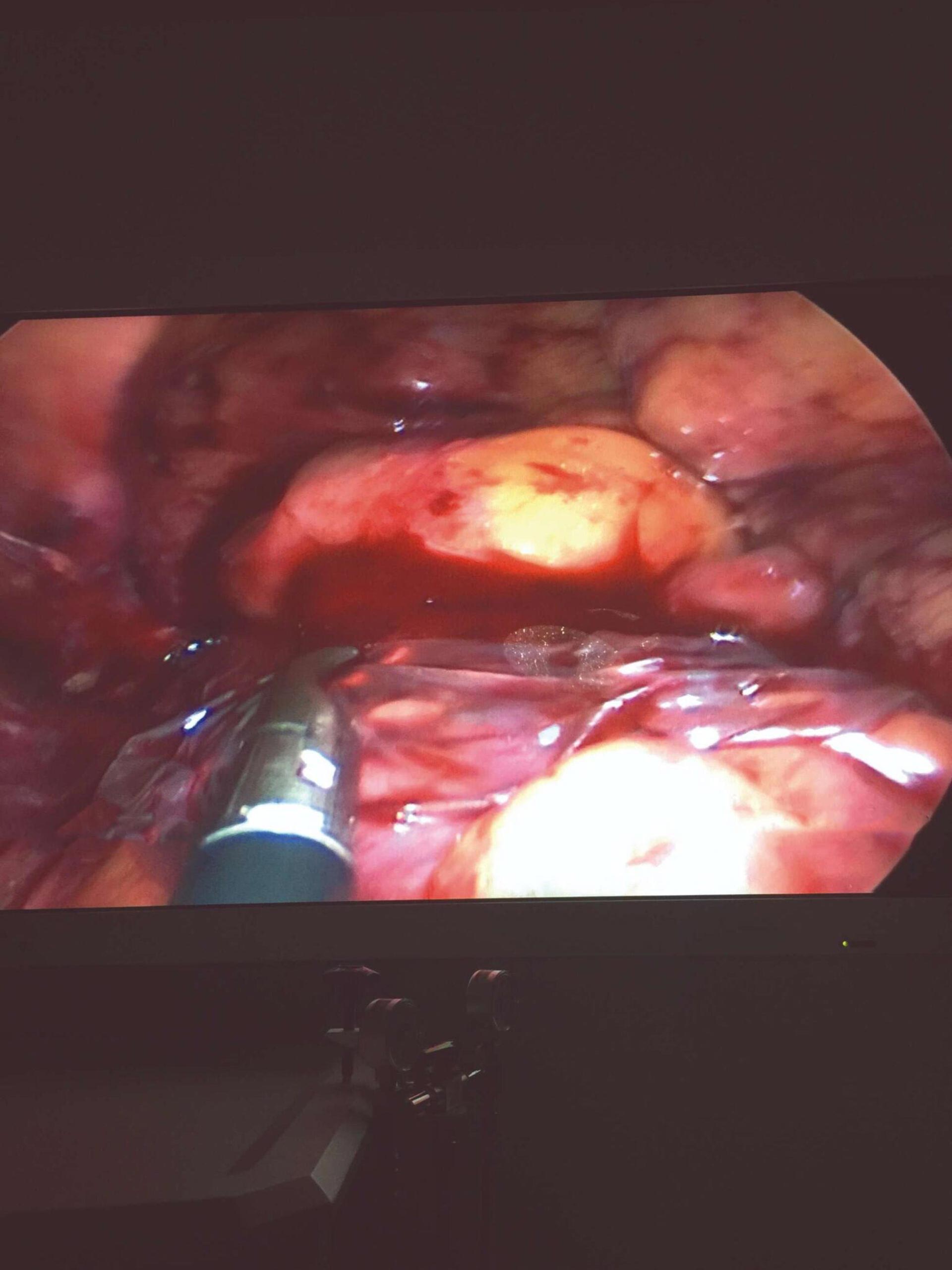
Colostomy Reversal with AMNIOFIX11
Challenge
A 68-year-old male underwent an emergency Hartmann’s procedure with a rectosigmoidectomy and end colostomy with a rectal pouch, due to a perforation of the sigmoid colon from acute diverticulitis. Though wound healing in elderly people is not necessarily impaired, age-related changes are evident. Comorbidities, which are associated with impaired healing, are more prevalent in older patient populations and can delay healing by 20-60%.12 Anastomotic leakage is the most common and much-feared intraoperative complication in colostomy reversal.13,14 One study showed the anastomotic leakage rate at as high as 3.8%.15 In addition to anastomotic leakage, other common postoperative complications include wound infection, incisional hernia, ileus, and enteric fistula formation.13,14
Surgical Intervention
Five months later, when the patient’s overall condition improved, a colostomy reversal using a single-port laparoscopic technique with AMNIOFIX was performed. A 2 cm x 6 cm AMNIOFIX graft was placed laparoscopically on the colorectal anastomotic stapled site and was stitched into place with absorbable sutures.
Follow-Up
The patient was seen two weeks after the surgery with no postoperative complications. The patient was having normal bowel movements daily.
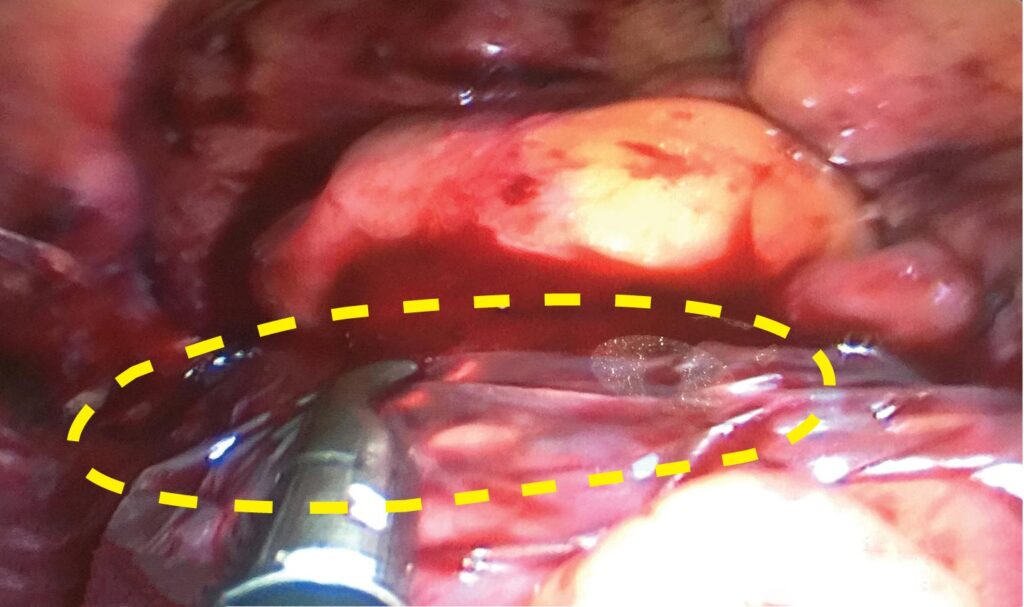 Single port laparoscopic approach |
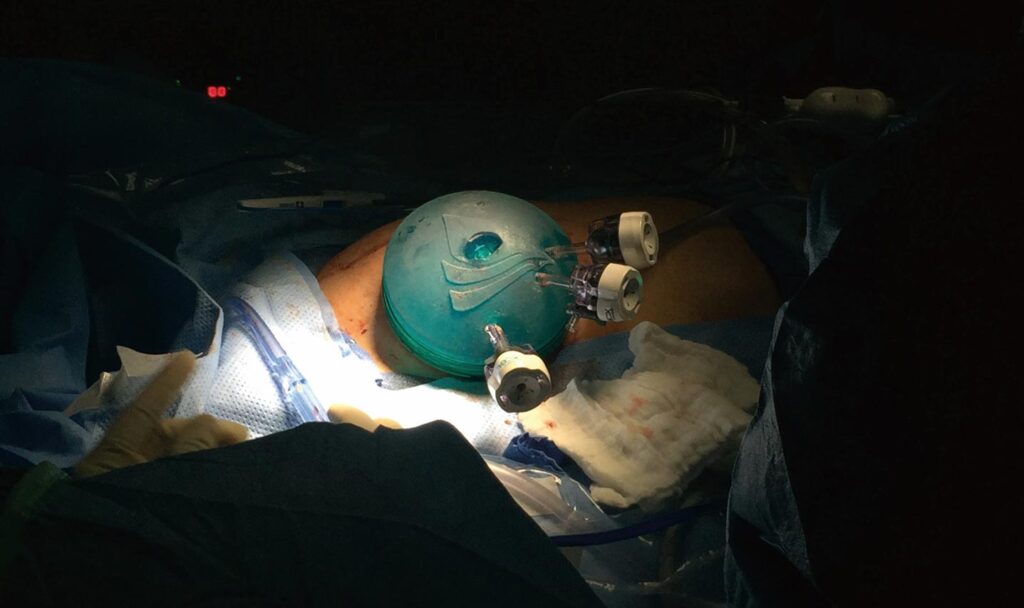 2 cm x 6 cm AMNIOFIX placed on anastomosis 2 cm x 6 cm AMNIOFIX placed on anastomosis |
clinical evidence
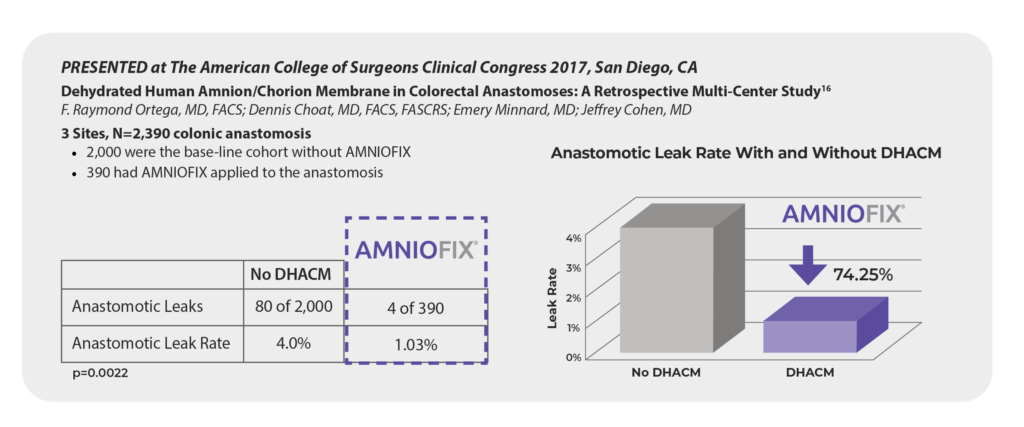
DHACM in Colorectal Anastomoses: A Retrospective Multi-Center Study16
Resources
General & Colorectal Surgery Casebook
General & Colorectal Surgery Casebook
MIMEDX offers a portfolio of advanced placental-based allografts in the surgical setting.
- AMNIOFIX®
- AMNIOCORD®
- AMNIOEFFECT®
- AMNIOBURN®
- AXIOFILL®
References
- Atkin L, Bućko Z, Conde Montero E, et al. Implementing TIMERS: the race against hard-to-heal wounds. J Wound Care. 2019;23(Sup3a):S1-S50.
- Koob TJ, Lim JJ, Massee M, Zabek N, Denozière G. Properties of dehydrated human amnion/chorion composite grafts: Implications for wound repair and soft tissue regeneration. J Biomed Mater Res B Appl Biomater. 2014;102(6):1353-1362.
- Lei J, Priddy LB, Lim JJ, Massee M, Koob TJ. Identification of Extracellular Matrix Components and Biological Factors in Micronized Dehydrated Human Amnion/Chorion Membrane. Adv Wound Care (New Rochelle). 2017;6(2):43-53.
- MIMEDX Internal Report. MM-RD-00086, Proteome Characterization of PURION Processed Dehydrated Human Amnion Chorion Membrane (dHACM) and PURION PLUS Processed Dehydrated Human Umbilical Cord (dHUC) Allografts.
- Bullard JD, Lei J, Lim JJ, Massee M, Fallon AM, Koob TJ. Evaluation of dehydrated human umbilical cord biological properties for wound care and soft tissue healing. J Biomed Mater Res B Appl Biomater. 2019;107(4):1035-1046.
- MIMEDX Internal Report. MM-RD-00113, Non-GLP Evaluation of Placental Based Products for Cellular Response in a Mouse Subcutaneous Implant.
- John Ko, MD, PhD, FACS, Plastic Surgery, Elmhurst, NY.
- Thombs BD, Singh VA, Halonen J, Diallo A, Milner SM. The effects of preexisting medical comorbidities on mortality and length of hospital stay in acute burn injury: evidence from a national sample of 31,338 adult patients. Ann Surg. 2007;245(4):629-634.
- Myles PS, Iacono GA, Hunt JO, et al. Risk of respiratory complications and wound infection in patients undergoing ambulatory surgery: smokers versus nonsmokers. Anesthesiology. 2002;97(4):842-847.
- Dunne JR, Malone DL, Tracy JK, Napolitano LM. Abdominal wall hernias: risk factors for infection and resource utilization. J Surg Res. 2003;111(1):78-84.
- Francis S. Lee MD, FACS, Quan Le, Christina W. Lee, General Surgery, Irvine, CA.
- Hammond J, Lim S, Wan Y, Gao X, Patkar A. The burden of gastrointestinal anastomotic leaks: an evaluation of clinical and economic outcomes. J Gastrointest Surg. 2014;18(6):1176-1185.
- Khan S, Alvi R, Awan Z, Haroon N. Morbidity of colostomy reversal. J Pak Med Assoc. 2016;66(9):1081-1083.
- Pittman DM, Smith LE. Complications of colostomy closure. Dis Colon Rectum. 1985;28(11):836-843.
- Kaiser AM, Israelit S, Klaristenfeld D, et al. Morbidity of ostomy takedown. J Gastrointest Surg. 2008;12(3):437-441.
- Ortega R, Choat D, Minnard E, Cohen J. Dehydrated Human Amnion/Chorion Membrane in Colorectal Anastomoses: A Retrospective Multi-Center Study. ACS Clinical Congress, October 22-26, 2017. San Diego, CA.